
September 11, 2024
Urinary Incontinence Diagnosis And Treatment

Urinary System Incontinence Medical Diagnosis And Treatment Urodynamically, both detrusor hyperreflexia and areflexia have actually been discovered. Roughly 40-70% of patients with Parkinson condition have lower urinary system disorder. Debate exists regarding whether particular neurologic issues in individuals with Parkinson illness bring about bladder disorder or if bladder signs just are related to aging. The extrapyramidal system is thought to have a repressive impact on the micturition center; in theory, loss of dopaminergic activity in this field might cause loss of detrusor inhibition. Some people with tension incontinence have urine leakage right into the proximal urethra that may, at first, trigger sensory necessity and/or bladder tightenings, which at first are suppressible.
Hrt For Prostate Cancer Cells Clients
What hormonal agent quits pee?
make less pee during the night. Takeaway: If progesterone levels are increasing during and after your cycle, and progesterone triggers your bladder to get extra often, it may cause urinary incontinence. Menstruation adjustments. There are lots of factors your regular monthly period can alter, but hormone discrepancy often plays a role.Hair problems.
Neurologic Reasons
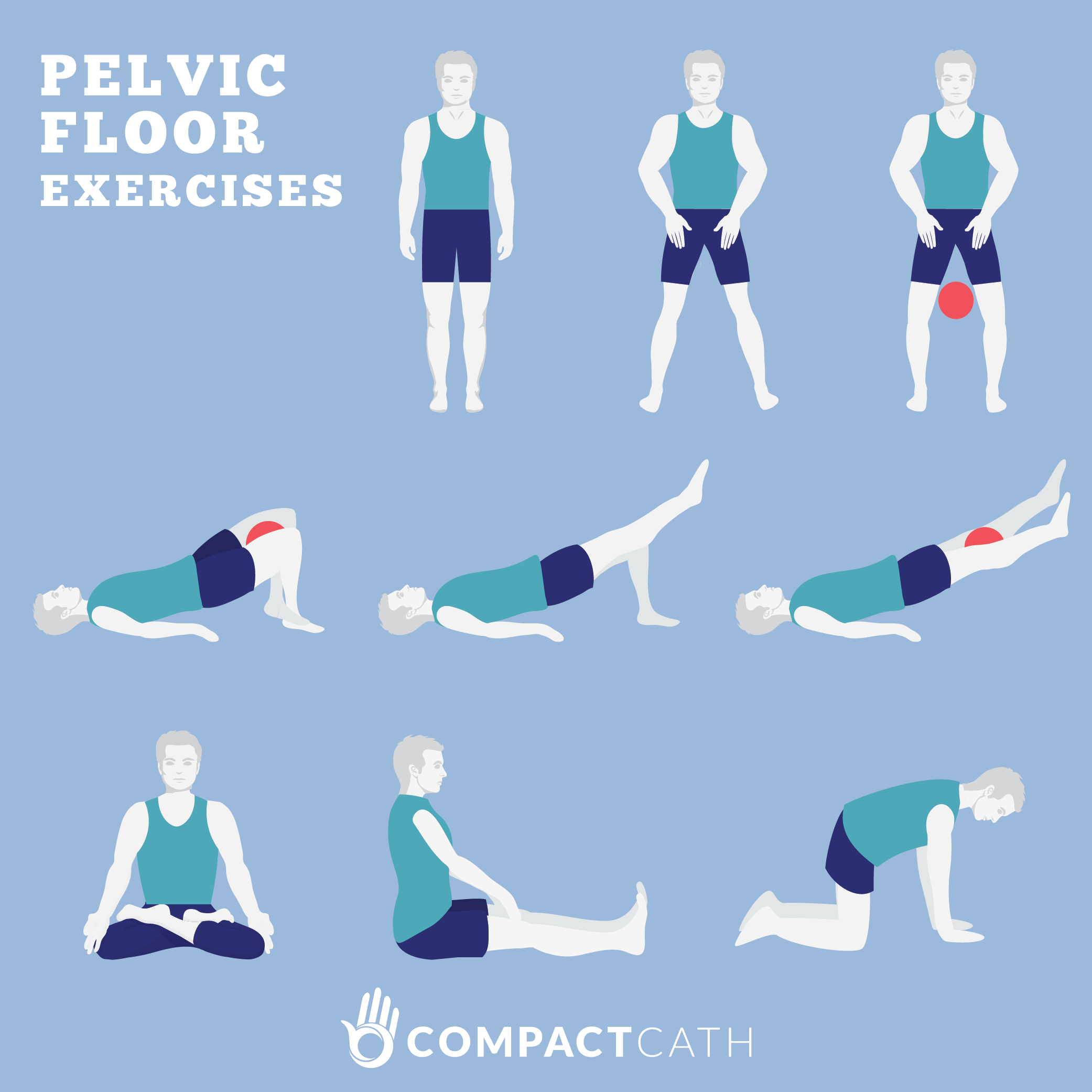
Low estrogen can trigger bladder signs by thinning the cells that lines the vagina. This reduces the elasticity and stamina of the vaginal canal and surrounding muscular tissues, lowering muscular tissue support for the bladder and related frameworks, such as the urethra. Nevertheless, not all individuals with reduced estrogen create bladder concerns. As an example, individuals who have formerly delivered may have pelvic flooring disorder.- Electrical treatments are used directly over the pelvic floor muscles.
- It's estimated half of women over age 65 have stress urinary incontinence.
- To help you determine and get the ideal muscles, your physician might suggest that you collaborate with a pelvic flooring physiotherapist or attempt psychophysiological feedback strategies.
- If a hidden problem is creating your symptoms, your medical professional will initially deal with that condition.
Social Links